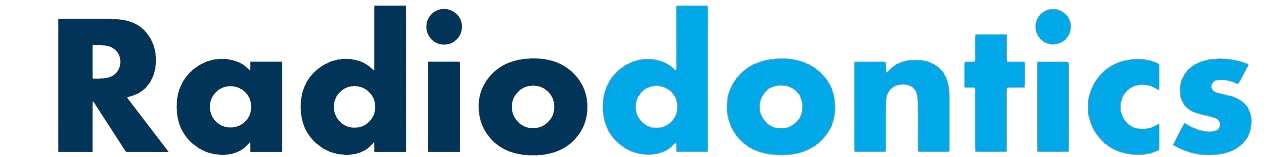
Periapical and Bitewing Radiopacities
Dr. Barett Andreasen, Oral and Maxillofacial Radiologist
Radiopacities will occasionally appear on a periapical or bitewing. This list of radiopacities that you may encounter serves as a starting point for your differential. It is not an exhaustive list but covers the vast majority of entities you will encounter as a dental professional. For radiopacities that are specifically at or near the root apex, please see our 'Apical Radiopacities' graphic.
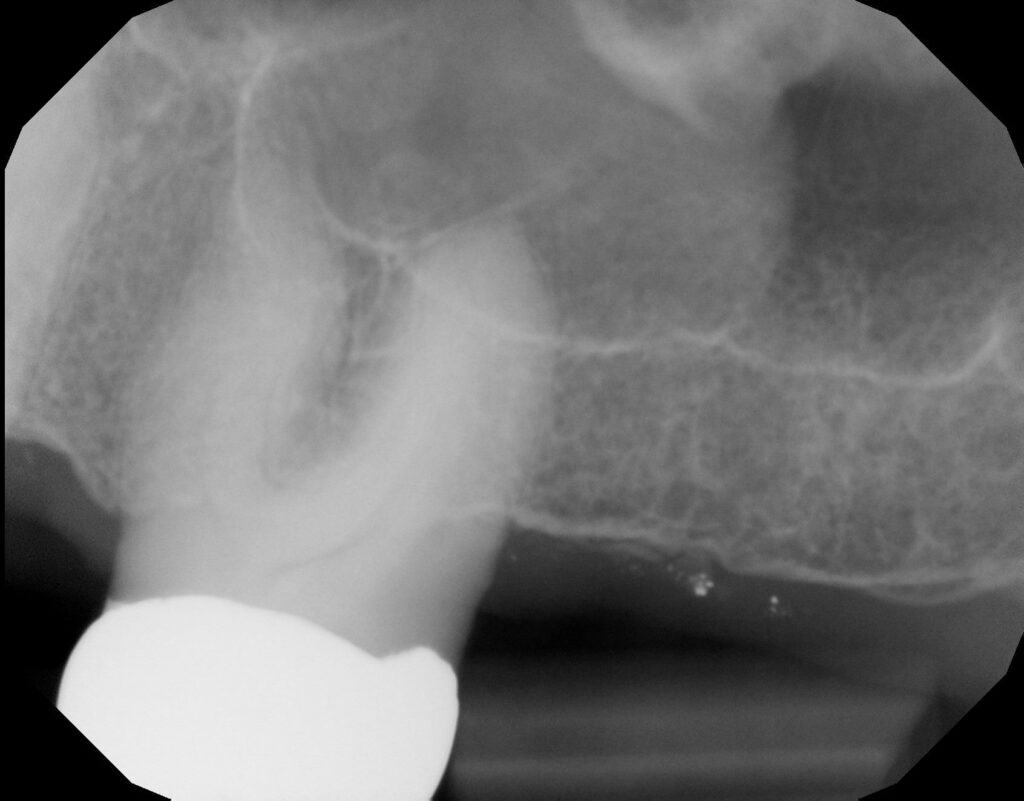
Antroliths
Antroliths appear as a calcified mass within the maxillary sinus separated from the adjacent sinus floor. Antroliths are often formed in the environment of chronic sinusitis and may originally calcify from a nidus of inflamed mucus, pus, clots or foreign bodies.
Antroliths present as a well-defined calcified mass, ranging from a faint to dense radiopacity with a laminated appearance, which may be difficult to appreciate on periapicals. They are roughly spherical or ovoid in shape and may be solitary or multiple in number.
No treatment for the antroliths themselves is necessary, if asymptomatic. However, the underlying cause for possible chronic sinusitis may need to be addressed. Treatment for chronic sinusitis can range from simple antibiotics to sinus surgery. Fungal sinusitis (aspergillosis) should be considered in cases that are unresponsive to therapy.
Osteomas
Osteomas are benign neoplasms of bone that can involve any part of the skeleton but are more commonly present in the craniofacial region. While more often found in the frontal and ethmoid sinuses, maxillary osteomas (sometimes called antral exostoses) can appear along the floor of the sinus in periapical radiographs. Radiographically, they appear as bony projections with a pedunculated, almost mushroom-like appearance. Other osteomas may have a broader, sessile base. The primary distinction between osteomas and antroliths is the relationship to the walls and floor of the sinuses - osteomas are directly connected to the floor or a wall of the sinus whereas antroliths are entirely separate from the floor of the sinus and are often 'floating' in thickened mucosa. On 2D imaging, osteomas often appear as homogenously dense radiopacities, though 3D radiography can reveal a more heterogenous (cancellous) center in some osteomas.
Generally osteomas are no cause for concern and require no treatment as long as the patient is asymptomatic and no sinus issues occur. However, when multiple osteomas are noted, the possibility of Gardner Syndrome should be ruled out.
Sialoliths
Formation of a mineralized mass within the salivary glands or ducts is termed a sialolith (salivary stone). Sialoliths arise from calcium deposits that form around a nidus within the duct lumen. Of the major salivary glands, the submandibular gland is most often involved, likely due to the upward and tortuous nature of the submandibular duct as well as its thicker, mucoid secretions.
On bitewings and periapicals, sialoliths present as a well-defined radiopacity that ranges from completely radiopaque to mixed-density in appearance. A lamellar or 'onion'-like appearance may be evident, reflecting the chronic and repeated deposition of calcium that forms these entities. Sialoliths are normally spherical or oval with smooth borders, but can be elongated if within a duct.
Patients may present with a history of recurrent swelling and/or pain during mealtimes, though many cases are asymptomatic. Stimulation of salivary flow, hydration, massage and moist heat can often dislodge smaller sialoliths. Larger stones may require surgical intervention, such as excision or sialoendoscopy.
Mucositis/Mucosal thickening
When the root apices of maxillary posterior teeth project through the maxillary sinus floor, apical periodontitis involving these teeth may produce a localized mucosal tissue edema termed periapical mucositis. This thickened mucosa can be evident on periapicals of the posterior maxillary teeth and appears as a soft tissue expansion (less radiopaque than bone) directly adjacent to the infected root apex.
Additionally, sinogenic mucosal thickening may be present along the floor of the maxillary sinuses. Mucosal thickening is not associated with apical inflammation but rather is due to localized inflammation within the sinus itself. This may be due to factors such as allergies, pollution, the common cold, dust or other conditions. The appearance of mucosal thickening is the same as mucositis - soft tissue density thickening at the floor of the sinus - but again is not of dental origin.
Neither mucositis nor mucosal thickening require treatment, though the offending tooth associated with the mucositis should obviously be addressed.
Mucous Retention Pseudocyst
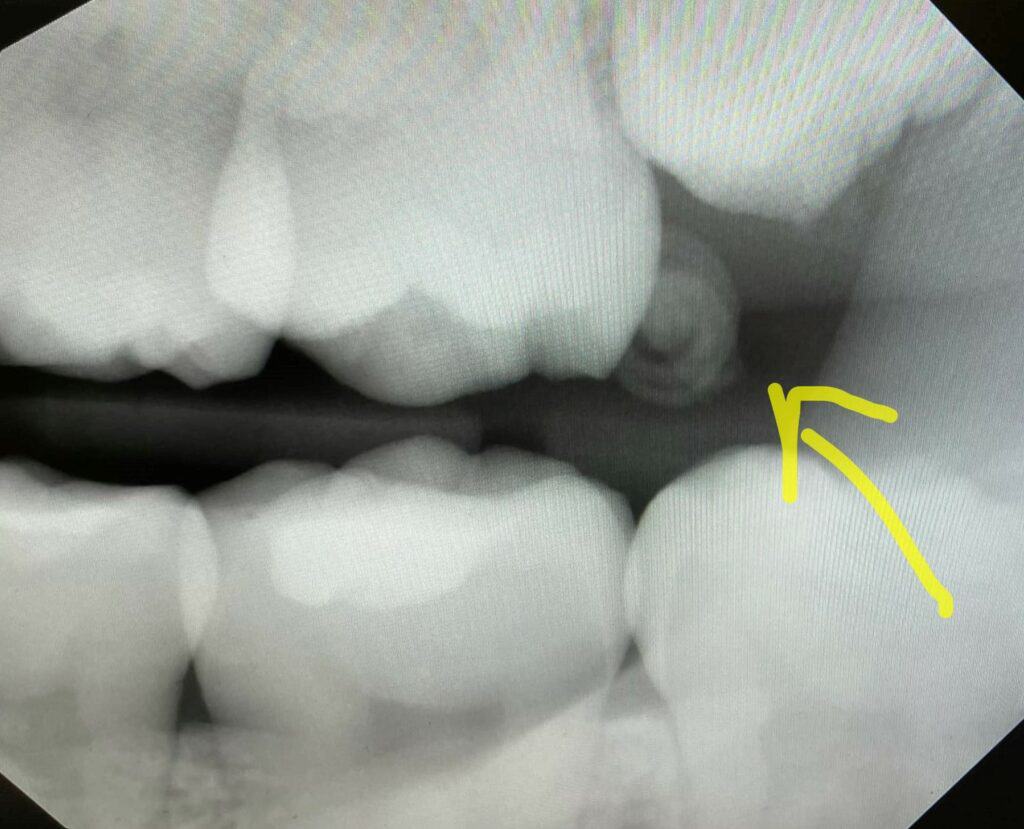
Mucous retention pseudocysts occur when submucosal mucinous glands within the paranasal sinuses become obstructed. This leads to an accumulation of fluid beneath the sinus mucosa and results in a swelling of the tissue.
The radiographic appearance of mucous retention pseudocysts is described as a dome-shaped radiopacity along the floor or wall of a sinus. The borders are well-defined and smooth but lack cortication. This is an important distinction as it helps distinguish mucous retention pseudocysts from pathology arising from the adjacent bone.
Mucous retention pseudocysts have no effect on the surrounding structures and as such, the borders of the involved sinus should always remain intact and without any expansion or displacement. If the pseudocyst is superimposed over the roots of a tooth, the lamina dura and PDL space should be unaffected.
No treatment is typically necessary for mucous retention pseudocysts as they normally cause no symptoms and resolve spontaneously without any surgical intervention.
Tori
Tori are outgrowths of bone typically composed of dense cortical bone arising from the buccal or lingual surfaces of the alveolar bone. These entities are often evident clinically and range from barely palpable masses to large bilateral outgrowths that contact near the midline.
Tori can be noted on periapical and bitewing radiographs and often appear as a ovoid radiopacity at or just apical to the alveolar crest. Most often, tori that appear on radiographs are located lingual to the mandibular premolars but maxillary tori can be seen as well.
Treatment for tori is unnecessary if asymptomatic (the thin mucosa over the tori is susceptible to trauma) and if removal is not needed for any planned prosthesis.
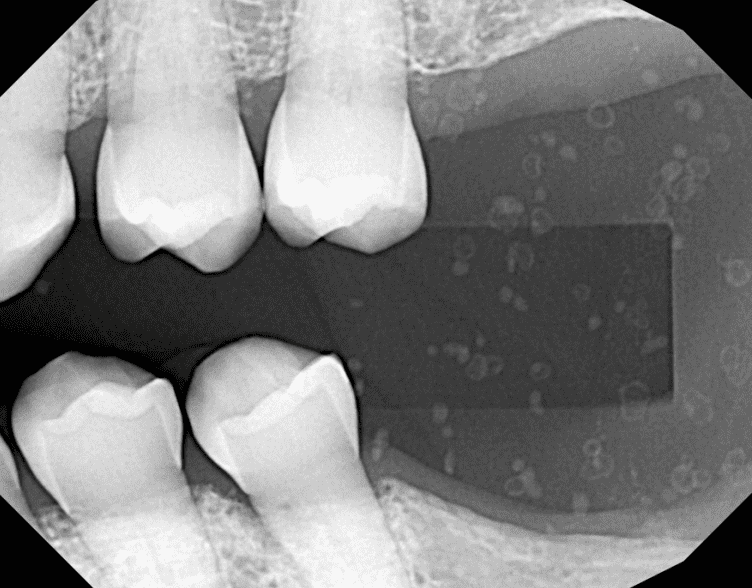
Osteoma Cutis
Osteoma cutis represents the formation of small calcified nodules in the facial skin. Approximately 85% of cases occur as a result of acne of long duration, developing in a scar or chronic inflammatory traumatic or neoplastic dermatosis. Cases of osteoma cutis are benign, noninvasive and typically asymptomatic in nature, though larger lesions may be palpated.
Osteoma cutis may occasionally be present on 2D imaging, most often on posterior bitewings. These cases typically present with multiple small, washer-shaped radiopacities in the soft tissues of the face. The internal structure may be radiolucent or more radiopaque depending on the degree of calcification.
No treatment is required but lesions may be removed due to cosmetic concerns.
Dense Bone Island
Also known as idiopathic osteosclerosis, enostosis, or hyperostosis, this finding is of unknown etiology and typically occurs in the posterior mandible. While often associated with the root apices of mandibular molars and premolars, it can be found anywhere within the jaws.
Dense bone islands present as a dense, homogenous radiopacity with an amorphous shape. When associated with a root, a regular PDL space is maintained and the tooth is vital. On a CBCT, it will blend into adjacent cortices with no thinning or expansion. These features help differentiate idiopathic osteosclerosis from similar entities such as condensing osteitis, cemento-osseous dysplasia, hypercementosis, and cementoblastoma.
No treatment is necessary for areas of idiopathic osteosclerosis.
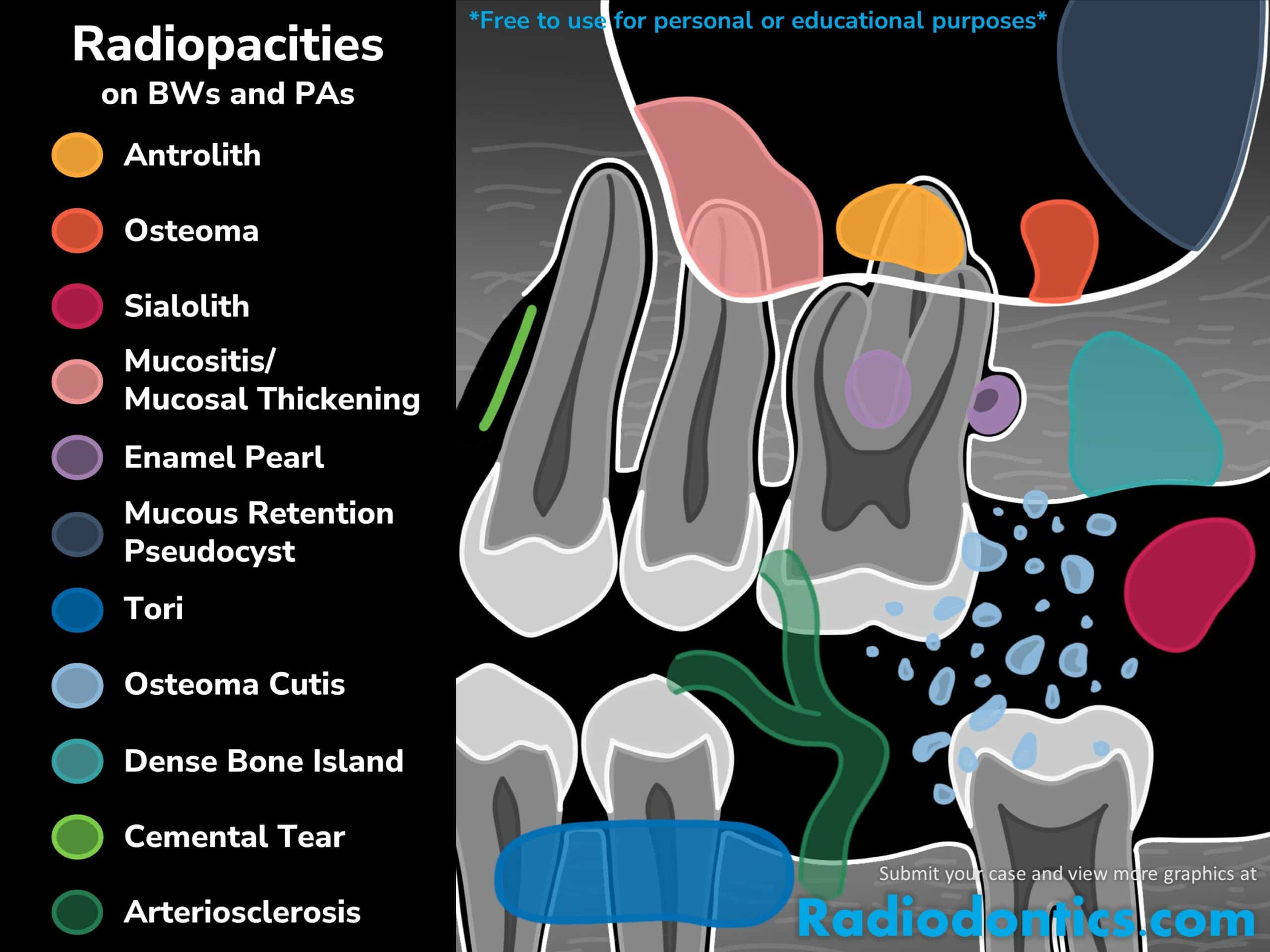
Enamel Pearl
The enamel pearl is a small formation of enamel approximately 1-3mm in diameter that occurs on the roots of molars. Most enamel pearls develop in the furcal areas of molar teeth, often at or just apical to the CEJ. Enamel pearls appear as smooth, round radiopacities, often with the same density of enamel found within the crown of the tooth.
No symptoms are typically associated with enamel pearls; however, depending on the location, enamel pearls may predispose to formation of a periodontal pocket and subsequent periodontal disease. Removal may be needed if this is the case.
Cemental Tear
A cemental tear is a special type of surface root fracture that may cause periodontal and/or periapical bone destruction. In a cemental tear, a layer of cementum is separated from the underlying root dentin as a result of excessive occlusal forces or trauma to the jaws. This sheared-off fragment remains within the periodontal ligament and acts as a constant irritant. On radiographs, this appears as a linear radiopacity that parallels the adjacent root surface. While usually completely separate, some fragments may remain attached to the root surface.
Cemental tears can present as part of apical periodontitis but can also occur independently with a vital pulp. Soft tissue swelling, localized periodontal pocket, periodontal/periapical bone loss are noted clinical characteristics of cemental tears.
Treatment options include nonsurgical scaling and root planing, surgical debridement with periodontal/apical surgery, surgical debridement combined with GTR and bone grafting, and extraction.
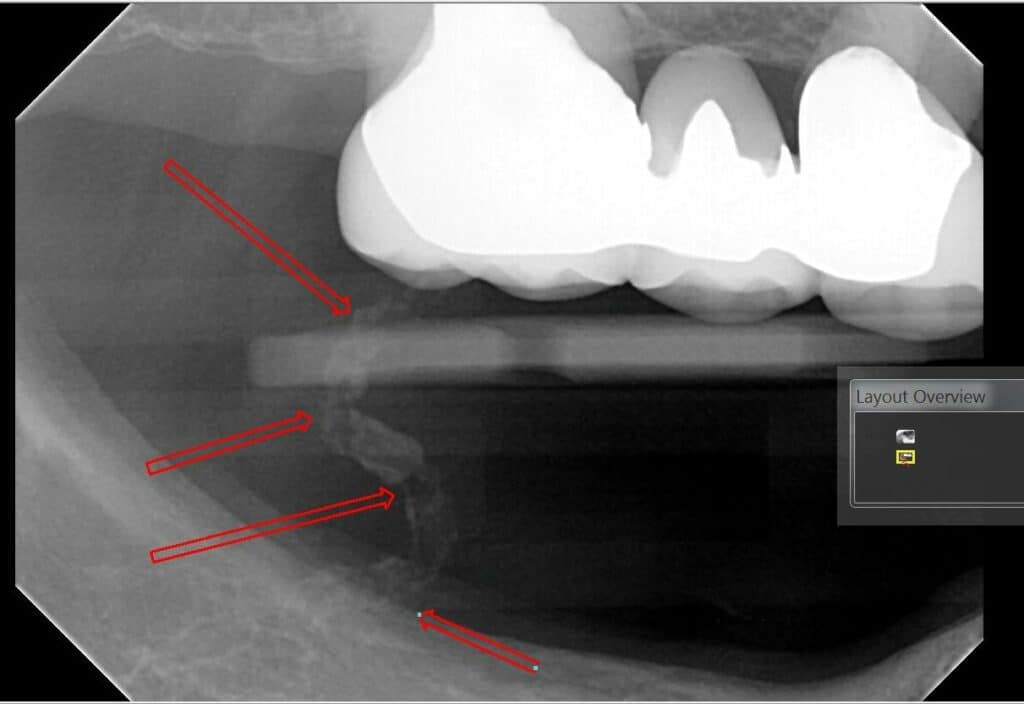
Arteriosclerosis
Degeneration and eventual loss of elastic fibers followed by deposition of calcium salts in the medial layer of an artery results in a condition called arteriosclerosis. This condition, also called Monckeberg's medial calcific sclerosis, which leads to a reduction in vessel elasticity and compliance. These calcifications can be seen involving the facial artery and the branches of the maxillary artery and may be imaged by bitewing and panoramic radiographs.
Calcifications of arteriosclerosis appear as 'train-track' radiopacities that follow the course of the artery. No treatment is needed for arteriosclerosis; however, correlation with the patient's medical history is highly recommended as these findings are typically noted in patients with uncontrolled diabetes and chronic renal disease.
A Word of Caution
There are, as always, exceptions to these rules. As anyone who practices in the field of dentistry knows, nothing ever quite follows the textbooks, especially when delving into the field of pathology and radiology. The entities covered above demonstrate many various presentations and manifestations which cannot be covered in this article, and that's not to mention the numerous pathologies which were not discussed.
If you have any questions about a radiograph, please send your case to Radiodontics by using the 'Upload Case' button at the top of the page to have your images be reviewed by an oral and maxillofacial radiologist.